Water-soluble vitamins
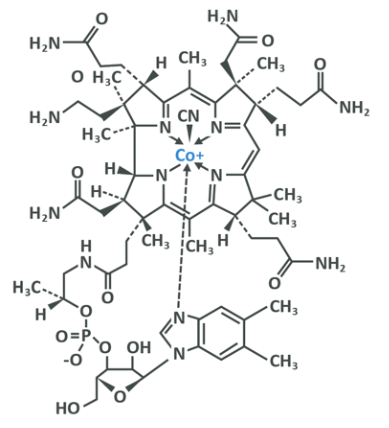
Water-soluble vitamins are water-soluble due to their molecular makeup. Unlike hydrophobic fat-soluble vitamins which have a non-polar structure, water-soluble vitamins have polar structures which means that atoms within them do indeed have an electromagnetic charge or a ‘polarity’ and this allows them to combine with the polar molecules which also make up water. The incredibly complex structure you see below is vitamin B12.
Water-soluble vitamins are digested via your small intestine straight into your blood much like amino acids and glucose. From here they are transported to the cells that need them, and excessive amounts in your blood are generally excreted readily in urine. There are no long-term storage sites for water-soluble vitamins – you either use them or they are removed.
This means that toxicity from overconsumption is almost impossible and side effects are non-existent outside of those seen from extremely high supplemental intakes which may cause gastric upset (such is the case for vitamin C). Unfortunately, this also means that if you consume a very low amount for a relatively long period, your body will not have any additional stores to ‘tap in to’. As such, daily intake is more important, and deficiency is a bit more of a realistic prospect.
The water-soluble vitamins can be further grouped together into the B vitamin complex and vitamin C. The B vitamins all have very similar functions in the body and are found in foods which have a lot of overlap between them, and as such have been historically considered together despite being chemically distinct. We will very briefly lay out the functions of the B vitamins, with the exception of B12 and folic acid which need to be considered in a little more detail, before covering vitamin C.
The B vitamins are all either cofactors or precursors to them, with the majority being co-enzymes. Co-enzymes, for example, are molecules which must be bound to an enzyme for that enzyme to be able to carry out the effect that it does, and as such the B vitamins can be considered generally to have the function of allowing cellular metabolism to occur efficiently.
Vitamin B1
Also known as thiamine. Needed as a coenzyme for the proper metabolism of pyruvate to acetyl CoA, meaning that it is key in the release of energy from glucose (the process of cellular respiration was covered in module 2). It’s also involved in proper DNA production and is needed for your nerves to work properly. Deficiency is seen in people with diets that rely on milled rice and raw fish (milled rice is void of these nutrients, and raw fish contains compounds which prevent absorption). As such, it is still endemic in Asia.
The only other situations outside of limited food consumption or cases of related health complaints where deficiency is likely is in exclusively breastfed infants whose mothers are deficient, or in chronic alcoholism.
Deficiency can lead to a disease called beriberi. The WHO RNI is 1.1mg for women and 1.2mg for men, 1.4mg for pregnant women and 1.5mg for those who are lactating. The current British recommendations are 1 and 0.8mg per day for men and women respectively. Toxicity is not possible due to extremely rapid excretion times for overconsumption.
Good sources include vegetables, eggs and whole grains.
Vitamin B2
Also known as riboflavin. Deficiency is incredibly uncommon outside of situations of severely limited food intakes, or other clinical or genetic issues which prevent absorption. Riboflavin is needed during the processes which produce energy including the electron transport chain which extracts ATP from NADH+.
Deficiency can lead to hypo or ariboflavinosis, categorised by a sore throat, bruising in the back of the throat, and issues with immune function. Toxicity is not possible due to limited intestinal absorption.
The WHO RNI is 1 and 1.3mg per day for females and males respectively, rising to 1.4mg for pregnant and 1.6mg for lactating women. In the UK the recommended intake is 1.3mg per day for men and 1.1mg per day for women. Good sources include milk, eggs and rice.
Vitamin B3
Also known as niacin. Niacin is used within respiration performed by cells and is also needed during the processes involved with DNA repair. Additionally, it’s needed in fatty acid and steroid synthesis. Deficiency can lead to a condition called Pallegra, which involves diarrhoea, dermatitis and dementia. If untreated this leads to death.
Toxicity is unlikely but possible, so taking extremely large doses should be avoided – the TUL for Niacin is 35mg per day. Taking a large dose can also lead to skin flushes and heat (therefore sweating and vascularity), which is why it’s often found in pre-workout supplements.
The WHO RNI for Niacin is 14 and 16 mg per day for women and men respectively, rising to 18 mg for pregnant and 17mg for lactating women. The UK recommended intakes are 13 and 17mg for women and men, respectively.
Good sources of Niacin include meat, fish, milk, wheat, sweet potatoes, squash, corn and eggs.
Vitamin B5
Also known as pantothenic acid. This is required for the oxidation of fatty acids and carbohydrates for energy due to its involvement with CoA. Deficiency is very unlikely, but can lead to postural hypotension, unusually elevated heart rate during exercise, constipation and hand and feet numbness.
Toxicity is unlikely.
The WHO RNI for B5 is 5mg per day for males and females, 6mg for pregnant women and 7mg for lactating women. The UK recommended intake is 5mg per day for both sexes.
Good sources include meat, poultry, green vegetables, sweet potato, cauliflower, eggs and wholegrains.
Vitamin B6
B6 is heavily involved in amino acid metabolism, steroid hormone breakdown and recycling, and energy production as well as haemoglobin synthesis (haemoglobin allows red blood cells to carry oxygen). Deficiency is extremely rare and symptoms are difficult to isolate as deficiency in B6 usually happens alongside deficiency in other nutrients. Immune function dysregulation, skin issues and potential decrease of brain glutamate metabolism are associated with extremely low intakes.
Deficiency is very, very rare, happening only in those on excessively restricted diets (it appears on eating disorder wards) or those who are on haemodialysis. Toxicity is rare, but symptoms of neurotoxicity have been observed in situations where very high dose B6 has been used in the treatment of pre-menstrual syndrome (PMS), carpal tunnel and some neurological conditions. As such a theoretical TUL of 100mg has been adopted.
The WHO RNI is 1.3mg for males and females, though this rises to 1.5 and 1.7mg for females and males respectively after age 50. In pregnant and lactating women, the numbers are 1.9 and 2mg respectively. The UK recommended intake level is 1.4mg for men and 1.2mg for women.
Good sources include vegetables, beans, peanuts, eggs, potatoes and milk.
Vitamin B7
Also known as biotin, this plays a vital role in the metabolism of all three macronutrients owing to its function as a coenzyme of critical carboxylases, which are enzymes that add COOH groups to things during metabolic reactions.
Deficiency can be seen in those who consume a large amount of raw eggs (raw eggs have biotin-binding proteins call avidin which block absorption), babies fed formulae which haven’t been properly formulated to contain enough nutrients and people with short-gut syndrome. Otherwise deficiency is very rare, though if it does occur it is detectable by dermatitis, conjunctivitis, alopecia, lethargy and developmental delays in infants.
Toxicity is not a problem due to limited intestinal absorption.
The WHO RNI for Biotin is 30ug per day for men and women including pregnant women, rising to 35ug during lactation. The UK the recommended intake is 30ug.
Good sources include eggs, almonds, cheese, mushrooms, sweet potatoes and spinach.
Vitamin B9
Also known as Folate, derivatives function in the transfer of carbon from donor molecules to others in metabolic reactions, and are used in DNA production, in the formation of the neurotransmitters that allow your nervous system to communicate, in the production of white cells and red blood cells and in amino acid metabolism.
Deficiency is surprisingly common, not least of all because the natural forms of folate are highly unstable and may become less active during harvesting, transport, storage, processing and cooking of foods. Synthetic supplemental folic acid is far more bioavailable and stable. Deficiency can lead to megaloblastic anaemia (enlarged red blood cells) and elevated levels of homocysteine (a by-product of other metabolic processes). Elevated homocysteine levels can lead to a number of issues including thrombosis and fractures.
Finally, a deficiency in folate present in pregnant women can lead to severe birth defects including spina bifida.
The WHO recommends 400ug per day for men and women, rising to 600ug in pregnant women and 500ug in those who are lactating. In the UK the recommended intake is 200ug per day.
The general recommendation is for women who are pregnant or planning on becoming pregnant take a 400ug folic acid supplement every day. Speak to your GP if you are, or are planning on becoming pregnant and they will be able to advise about this.
Good food sources include dark green leafy vegetables, flaxseeds, mango and avocado, though a lot of dietary folate is consumed via fortified cereals and breads.
It’s unlikely that dietary folate intakes would ever reach toxicity, but supplemental folic acid should not be taken in amounts over 1mg. In fact, doses of higher than 1mg can disguise deficiency of vitamin B12 because elevated folate levels can reduce the size of the megaloblastic red blood cells caused by B12 deficiency. This is a potential issue for those susceptible.
Vitamin B12
B12 aids folate in cellular reproduction. B12 is also crucial in homocysteine utilisation and metabolism and it is essential to the production of healthy red blood cells. A deficiency of vitamin B12 can lead to subacute combined degeneration which is a permanent and debilitating degeneration of the posterior and lateral columns of the spinal cord. This results in loss of function in extremities, cognitive issues and worse.
Alongside this B12 deficiency can lead to megaloblastic anaemia and the associated weakness and fatigue. This can be masked by excessive folate intake, which will then leave the former condition to manifest unbeknownst to the individual until it is too late, which is an all-too stark reminder to be careful when super-dosing vitamins or consuming an unbalanced diet.
B12 is extremely well-sourced from animal products, but there are no plants which synthesise it meaning that vegans are at severe risk of deficiency. Marmite, kimchi and some other fermented foods are the only vegan sources and therefore, unless these are eaten daily, a vegan should supplement with this nutrient.
The WHO RNI is 2.4ug per day for men and women, rising to 2.6ug for pregnant and 2.8ug for lactating women. The UK recommended intake is 1.5ug per day. Excessive intake will not cause toxicity as excretion is very rapid.
Good sources include almost animal products including eggs and dairy, fortified breakfast cereals and marmite.
Vitamin C
Also known as ascorbic acid. Its main role is as an antioxidant, though it is also used in collagen synthesis. It also enhances iron uptake and thus is frequently prescribed with iron supplements. 25mg of vitamin C with meals can increase iron availability by 65% (this is present in a very small serving of most vegetables) and therefore those supplementing with iron should take this with meals.
Vitamin C is necessary for collagen synthesis and production, so it can be very important in recovery and injury cases as collagen is a key ‘ingredient’ in connective tissue. Extreme deficiency is well known for causing the excessive bleeding condition known as scurvy, categorised by bleeding gums, loose teeth and bruising.
Although vitamin C is useful for fighting off illness, there is no good evidence to suggest that super-dosing it is good for reducing cold symptoms, and it’s unlikely that consuming a large amount improves injury recovery due to rapid excretion times after overconsumption. In fact, large-doses of vitamin C can cause GI distress.
The WHO RNI is 45mg per day, rising to 55mg and 75mg for pregnant and lactating women respectively. The UK recommended intake is 40mg. The suggested TUL is 1000mg.
Good food sources include citrus fruits, peppers, berries, dark green leafy vegetables, white potatoes and blackcurrants.