The SCN
Evidence for the fact that the human sleep/wake cycle is innately controlled comes from studies in participants who live for the duration of the experiment in an environment removed from external cues. It would be very easy to argue, for example, that we wake and sleep according only to light conditions or temperature but that does not seem to be the case. In these experiments caves or bunkers are often used to remove all natural light or temperature interference.
In one such study participants underwent a 5 day period of living in dim artificial light which included radio or TV usage, thus allowing them to have some temporal cues as to the time, and when this was the case they maintained a 24 hour sleep/wake cycle. After these cues were removed the subjects started to awaken later in the day and each whole cycle started to last around 28 hours rather than the usual 24, but it still seemed that the subjects lived in a rhythmic fashion and when cues were restored they reverted to a 24 hour cycle almost immediately. This indicates that a cyclical process is occurring but it is imperfect in isolation as we will discuss later. Below is a graph which shows their sleep/wake periods according to the availability of temporal cues (the blue arrow on each line is an indication of rectal temperature – remember that it’s not only waking and sleeping which is controlled by a circadian rhythm).
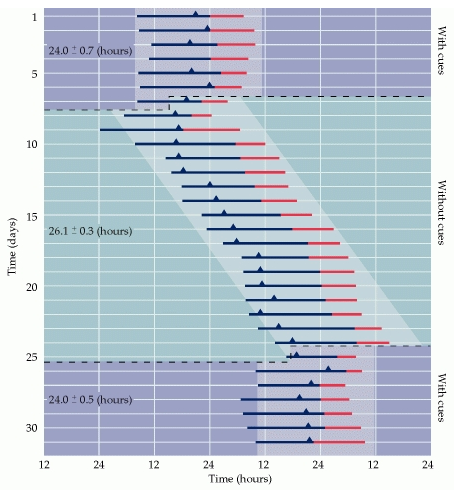
(Image taken from Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Neuroscience. 2nd edition. Sunderland (MA): Sinauer Associates; 2001. The Circadian Cycle of Sleep and Wakefulness. Available from: https://www.ncbi.nlm.nih.gov/books/NBK10839/).
Many regions in your body are operating in a rhythmic fashion, and researcher’s hypothesise that every single cell within your body has some amount of rhythmic action, varying hour-to-hour over a given period. As a result, your heart, liver, digestive tract and many other areas all ‘know’ when it’s night or daytime, but if this was left unchecked and able to run freely it would mean that trillions of clocks would need to line up independently – somewhat unlikely, so what’s controlling it all? Deep inside your brain is one of the oldest parts, evolutionarily speaking – the hypothalamus. This area is responsible for an enormous amount of our major functions by being the area which can connect your nervous system to your endocrine system. For example, in order for your body to release the hormone cortisol, the hypothalamus receives a signal from your nervous system then sends a signal to the pituitary gland, which in turn signals your adrenal glands, which ultimately secrete cortisol into the bloodstream.
Inside this brain region, close to the optic nerve are two small areas totalling around 20,000 neurons called the suprachiasmatic nuclei (SCN), and it is this area that is referred to as your ‘master body clock’. This is an example of an oscillator which is distinct from the usual homeostatic mechanisms about which we have spoken so far. A homeostatically regulated system always tries to fight to return to or stay at a predefined ideal, but an oscillator instead attempts to move towards something in particular. An example of a homeostatic system is a thermostat which turns on heating when the temperature drops but an example of an oscillator is a clock on your wall, always moving in one direction. So how does this group of neurons perform this task?
The neurons in the SCN are able to maintain their 24 hour cycle independently of each other and your body. When isolated and placed in a culture in a lab, a single SCN neuron will create spontaneous action potentials at predictable times of day despite being disassociated from any other neurons or other bodily systems, which means that these action potentials are created within the SCN itself. The way that these neurons are able to do this comes down to a gene expression feedback loop.
In the nucleus of the neuron, like that of every other cell, is a complete copy of your DNA. On that DNA are nucleotides in a particular order, with certain sections of nucleotides being called genes. These genes can do a number of things, one of which being coding for proteins. 2 proteins which are coded for by genes expressed within the nucleus of SCN neurons are PER proteins and CRY proteins. Two other proteins known as BMAL1 and CLOCK bind together and enter the nucleus of the cell to promote the transcription of PER and CRY genes. The resultant PER and CRY proteins combine to create a dipepdide which enters the nucleus and inhibits the action of BMAL1 and CLOCK, thus preventing its own expression. As PER and CRY build-up, their transcription decreases until you end up with a lot of PER and CRY but very little synthesis.
Over time, the PER:CRY complex degrades and allows CLOCK and BMAL1 to start to do their job again. This whole cycle takes around 24 hours and this is the molecular central bodily clock. The SCN then uses various signals to communicate with other areas of the body, aligning the clock that each of those has. It’s not that the SCN actively makes your heart beat differently at day and night, it’s the case that the SCN tells your heart when day and night is so that it’s able to change its beating pattern accordingly. When the SCN is removed or damaged, peripheral structures still display a rhythmic pattern of activity but they are all dis-regulated.
Furthermore, alterations in the genes which code for these proteins (amongst others) are what drive some people to be morning people or evening people. This is not due to laziness, preference or practice – it is simply the case that some people operate better or worse around 2 hours later or earlier than others.
The SCN is obviously manipulated by certain inputs. If this was set in stone you would not be able to recover from jet lag and you would not be able to alter your sleeping pattern according to different times of year or perhaps different working conditions requiring you to stay awake during the night. The wake/sleep circadian rhythm and more broadly the action of the SCN are entrainable owing to their sensitivity to light exposure.
The SCN receives information from your retina. Until recently it was thought that your eyes contained only rods and cones, as these are the photosensitive cells which can translate light energy into visual information, but studies using completely blind individuals indicated that the ability of a person to visually experience light was not a prerequisite for this. Rather, specialised light-sensing, non-visual cells on your retina translate light into information which is used by the SCN to calibrate to the day/night conditions in a given location. The removal of this calibration is why the individuals in the experiment above found that their sleep/wake cycle became dis-regulated.
Coming back to focus only on sleep – how is it that the SCN controls the sleep/wake cycle? The SCN calibrates to the current daytime/night time cycle and then signals for the pineal gland, a small, pinecone-shaped endocrine gland in the brain, to produce melatonin which has a sleep-promoting effect, but also, via a number of cascades, impacts on various other phenomena influenced by circadian rhythms including immune function, antioxidant defence action and glucose metabolism. Though the exact mechanism for this action of melatonin remains to be comprehensively elucidated, the fact remains that melatonin secretion corresponds precisely to the onset of sleep, while reduced melatonin secretion corresponds with wakefulness. Not only this, but impaired melatonin secretion is associated with insomnia while exogenous melatonin can induce sleepfulness.
Please note that it is not only melatonin involved in sleep. Many other neurotransmitters and hormones (remember, the difference between a neurotransmitter and a hormone isn’t within the chemical itself but the location of it – neurotransmitters impact neurons, hormones impact other cells, so some chemicals are both) are involved in sleep and wakefulness. The full extent of this is beyond the scope of this manual, but briefly:
- Glutamate is the most commonly found neurotransmitter in the brain, and the primary excitatory neurotransmitter, meaning that it ‘activates’ neurons and promotes the production of action potentials. Glutamate seems to regulate sleep duration to some degree, but it can also be converted into the following chemical (GABA)
- A neurotransmitter known as GABA is released to suppress action in the posterior hypothalamus. This area is responsible for wakefulness and so GABA secretion correlates with the onset of sleep
- The neurotransmitter orexin, produced in the hypothalamus, seems responsible for the regulation of many different aspects of sleep including processes involving dopamine, noradrenaline, histamine and acetylcholine. An impairment of orexin production is responsible for a lot of instances of the sleep disorder narcolepsy, which sees people becoming overwhelmingly tired at seemingly random parts of the day
- Dopamine, the ‘reward’ neurotransmitter, seems to regulate sleep/wake cycles, potentially by downregulating melatonin
- Acetylcholine seems to be important for REM sleep. The areas in which it is used as a key neurotransmitter are associated with the onset of REM sleep, and it’s highest overall during REM and wakefulness, but lowest during non-REM sleep
- Noradrenaline and serotonin both act to instigate wakefulness in the morning, working to increase and then maintain arousal and cortical function
- Cortisol is often referred to as ‘the stress hormone’ as it is released from the adrenal glands (small glands sitting on top of (ad-) your kidneys (-renal) in response to stressful situations. Cortisol’s main role is to promote glycogenolysis, lipolysis and protein breakdown to release glucose, fatty acids and amino acids into the bloodstream to use during a fight or flight scenario. Cortisol, however, is also partly responsible for waking you up in the morning. The usual secretion pattern for cortisol is to be high in the morning and then progressively reduce during the day until sleep, of course intermittently spiking in accordance with stress, exercise and other stimuli in between
- Growth Hormone Releasing Hormone’s (GHRH) main role, as the name suggests, is to promote the release of Growth Hormone (GH). It’s released during sleep and correlates to deep sleep. GHRH promotes this deep sleep, but it’s product, GH, can also help to maintain normal structure and metabolism. GH deficiency can lead to muscle loss and a relatively higher level of fat mass than is seen in individuals who have healthy GH production and though poor sleep is unlikely to cause clinically low GH secretion this is worth consideration
In sum, the SCN regulates the internal clock of every cell within your body via interactions with various endocrine structures including but not exclusively the pineal gland, which releases melatonin around the time that it starts to get dark and the adrenal glands which promote the release of cortisol to instigate wakefulness. The way that this is calibrated is through specialised retinal cells which are able to relay information about light conditions to the SCN, but the SCN itself is self-regulatory to some degree also.
Though this is fascinating and it answers a lot of questions it still leaves a few unanswered.
If sleep is regulated solely through circadian rhythms, why is it that after a few days of reduced sleep you feel the need to catch up? If it’s only circadian rhythms why is it that after a particularly difficult day you sleep much more deeply or for longer? Let’s look at the other, perhaps more intuitive mechanism for the manifestation of sleep.